Clinical examination
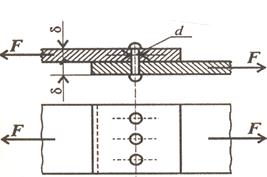
The indications for closed versus open reduction have changed dramatically over the last century. The ability to treat fractures with open reduction and rigid internal fixation (ORIF) has dramatically revolutionized the approach to mandibular fractures. Traditionally, closed reduction (CR) and ORIF with wire osteosynthesis have required an average of 6 weeks of immobilization mandibular fracture (IMF) for satisfactory healing. Difficulties associated with this extended period of immobilization include airway problems, poor nutrition, weight loss, poor hygiene, phonation difficulties, insomnia, social inconvenience, patient discomfort, work loss, and difficulty recovering normal range of jaw function. In contrast, rigid and semirigid fixation of mandible fractures allow early mobilization and restoration of jaw function, airway control, improved nutritional status, improved speech, better oral hygiene, patient comfort, and an earlier return to the workplace. The technique of rigid internal fixation was developed and popularized by AO/ASIF (Arbeitsgemeinshcaft fur Osteosynthesefragen/Association for the Study of Internal Fixation) in Europe in the 1970s. The basic principles of the AO, outlined by Spiessl, call for primary bone healing under conditions of absolute stability. Rigid internal fixation must neutralize all forces - tension, compression, torsion, and shearing - developed during functional loading of the mandible to allow for immediate function. This is accomplished by interfragmentary compression plates. Use an inferior border plate to counter compression forces and a superior border plate or arch bars to counter traction or tension forces at the superior border. AO reconstruction plates also impacted the management of comminuted and infected mandibular fractures. Ellis reported a 7.5% infection rate in treatment of mandibular angle fractures with and AO reconstruction plate without IMF. During the same time that Spiessl was expounding the AO doctrine, Champy et al in France was developing the concept of adaptive osteosynthesis. Champy advocated transoral placement of small, thin, malleable stainless steel miniplates with monocortical screws along an ideal osteosynthesis line of the mandible. Champy believed that compression plates were unnecessary due to masticatory forces that produce a natural strain of compression along the inferior border. These two changes of AO rigid internal fixation and the Champy method of monocortical miniplates revolutionized the treatment approach to mandibular fractures. Many fractures previously treated with closed reduction or open reduction with wire osteosynthesis are now commonly treated with open reduction with plate and screw fixation. An example of this evolution is the treatment of comminuted mandibular fractures. These were thought to be treated best by closed reduction to minimize stripping of the periosteum of small bone fragments. Although this treatment modality is still used, rigid fixation now enables the clinician to avoid closed reduction with the use of reconstruction plates and good soft tissue coverage.
|