Drug Excretion
The main route of drug excretion is through the kidney; however, volatile and gaseous agents are excreted by the lungs. Small quantities of drugs may pass into sweat, saliva, and human milk, the latter being potentially important in breast–feeding mothers. Although some drugs are excreted mainly unchanged into the urine, most are metabolized first. The first stage in excretion involves passive filtration of plasma through structures in the kidney called glomeruli, through which drug molecules pass freely. The drug thus reaches the renal tubule, where it may be actively or passively reabsorbed, or it may pass through into the urine. Many factors affect the rate of renal excretion of drugs, important ones being binding on plasma proteins (which impedes their passage through the glomerular filter) and urinary acidity, which can affect the rate of passive reabsorption of the drug by altering the state of its ionization. Renal drug excretion is the major route of drug elimination for polar drugs, water–soluble drugs, drugs with low molecular weight, or drugs that are biotransformed slowly. Renal clearance is the volume of drug contained in the plasma that is removed by the kidney per unit of time. Units for renal clearance are expressed in volume per time (e.g. milliliters per minute or liters per hour). Hepatic clearance is the volume of drug–containing plasma that is cleared by the liver per unit of time. Hepatic clearance is usually measured indirectly, as the difference between total body clearance and renal clearance, as shown in the following equation: Clh = Clт – ClR, where Clт is the total body clearance, and ClR is renal clearance. Blood flow, intrinsic clearance, and protein binding affect hepatic clearance. Blood flow to the liver is approximately 1.5 L/min and may be altered by exercise, disease, nutrition, or drugs. Blood enters the liver through the hepatic portal vein and hepatic artery, and leaves through the hepatic vein. After oral drug administration, the drug is absorbed from the gastrointestinal tract into the mesenteric vessels and passes through the hepatic portal vein and the liver into systemic circulation. Intrinsic clearance is based on the ability of the liver to remove the drug independently of blood flow. Intrinsic drug clearance primarily occurs due to the inherent ability of the biotransformation enzymes (mixed function oxidases) to metabolize the drug as it enters the liver. Biliary drug excretion, an active transport process, is also included in hepatic clearance. Separate excretion systems exist for weak acids and weak bases. Drugs that are excreted in bile are usually high–molecular–weight compounds or polar drugs such as reserpine, digoxin, and various glucoronide conjugates. Drugs may be recycled by the enterohepatic circulation. Some drugs are absorbed from the gastrointestinal tract through the mesenteric and hepatic portal veins, and proceed to the liver. The liver may secrete some of the drugs unchanged, or as a glucoronide metabolite, into the bile. From the bile (stored in the gallbladder), the drug may pass into the gastrointestinal tract through the bile duct. Presystemic elimination first–pass effects occur when the drug is administered orally. A portion of the drug is eliminated before systemic absorption occurs. First–pass effects generally result from rapid drug biotransformation by the liver enzymes. Other mechanisms include metabolism of the drug by gastrointestinal mucosal cells, intestinal flora, or biliary secretion.
II.13. Прочтите текст С и назовите пути выведения лекарств из организма. II.14. Назовите факторы, влияющие на печеночный клиренс. II.15. Расшифруйте по–английски эту формулу. Clh = Clт – ClR
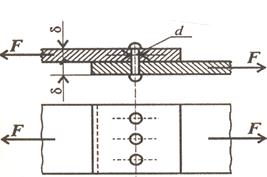
II.16. Заполните пустые клетки в этой схеме.
|