Read the text. A cochlear implant (CI) is a surgically implanted electronic device that provides a sense of sound to a person who is profoundly deaf or severely hard of
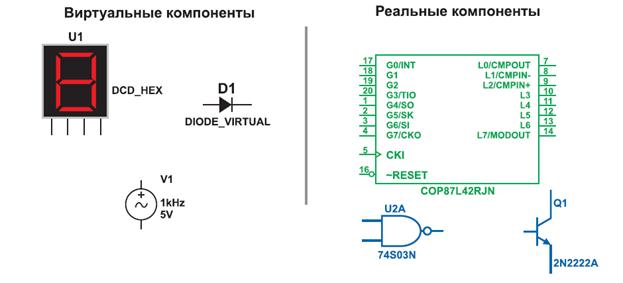
A cochlear implant (CI) is a surgically implanted electronic device that provides a sense of sound to a person who is profoundly deaf or severely hard of hearing. The cochlear implant is often referred to as a bionic ear. Cochlear implants can restore hearing in patients suffering deafness due to loss of sensory hair cells in their cochlea. In those patients, they can often restore sufficient hearing to allow unaided understanding of speech in a quiet background, but the restored, electrical hearing is much less rich than natural hearing, and offers only very limited appreciation of musical melody, or speech understanding in noisy environments. The discovery that electrical stimulation in the auditory system can create a perception of sound occurred around 1790, when Alessandro Volta (the developer of the electric battery) placed metal rods in his own ears and connected them to a 50-volt circuit, experiencing a jolt and hearing a noise " like a thick boiling soup". Other experiments occurred sporadically, until electrical (sound-amplifying) hearing aids began to be developed in earnest in the 20th century. The first direct stimulation of an acoustic nerve with an electrode was performed in the 1950s by the French-Algerian surgeons André Djourno and Charles Eyriè s. They placed wires on nerves exposed during an operation, and reported that the patient heard sounds like " a roulette wheel" and " a cricket" when a current was applied. The first attempt to develop a clinical CI was in 1957 by Djourno and Eyriè s. A recipient was implanted with a single channel device. The implant is surgically placed under the skin behind the ear. The basic parts of the device include: External: one or more microphones which picks up sound from the environment a speech processor which selectively filters sound to prioritize audible speech splits the sound into channels and sends the electrical sound signals through a thin cable to the transmitter, a transmitter, which is a coil held in position by a magnet placed behind the external ear, and transmits power and the processed sound signals to the internal device by electromagnetic induction, Internal:
The internal part of a cochlear implant. a receiver and stimulator secured in bone beneath the skin, which converts the signals into electric impulses and sends them through an internal cable to electrodes, an array of up to 24 electrodes wound through the cochlea, which send the impulses to the nerves in the scala tympani and then directly to the brain through the auditory nerve system. There are a number of factors that determine the degree of success to expect from the operation and the device itself. Cochlear implant centers determine implant candidacy on an individual basis and take into account a person's hearing history, cause of hearing loss, amount of residual hearing, speech recognition ability, health status, and family commitment to aural habilitation/rehabilitation. A prime candidate is described as: having severe to profound sensorineural hearing impairment in both ears. having a functioning auditory nerve having lived at least a short amount of time without hearing (approximately 70+ decibel hearing loss, on average) having good speech, language, and communication skills, or in the case of infants and young children, having a family willing to work toward speech and language skills with therapy not benefitting enough from other kinds of hearing aids, including latest models of high power hearing instruments and FM systems having no medical reason to avoid surgery living in or desiring to live in the " hearing world" having realistic expectations about results having the support of family and friends having appropriate services set up for post-cochlear implant aural rehabilitation (through a speech language pathologist, deaf educator, or auditory verbal therapist). People with mild or moderate sensorineural hearing loss are generally not candidates for cochlear implantation. Their needs can often be met with hearing aids alone or hearing aids with an FM system. After the implant is put into place, sound no longer travels via the ear canal and middle ear but will be picked up by a microphone and sent through the device's speech processor to the implant's electrodes inside the cochlea. Thus, most candidates have been diagnosed with profound sensorineural hearing loss. The presence of auditory nerve fibers is essential to the functioning of the device: if these are damaged to such an extent that they cannot receive electrical stimuli, the implant will not work. A small number of individuals with severe auditory neuropathy may also benefit from cochlear implants. A cochlear implant will not cure deafness or hearing impairment, but is a prosthetic substitute for hearing. Some recipients find them very effective, others somewhat effective and some feel worse overall with the implant than without. For people already functional in spoken language who lose their hearing, cochlear implants can be a great help in restoring functional comprehension of speech, especially if they have only lost their hearing for a short time. Individuals who have acquired deafblindness (loss of hearing and vision combined) may find cochlear implants a radical improvement in their daily lives. It may provide them with more information for safety, communication, balance, orientation and mobility and promote interaction within their environment and with other people, reducing isolation. Having more auditory information than they may be familiar with may provide them with sensory information that will help them become more independent. Some effects of implantation are irreversible; while the device promises to provide new sound information for a recipient, the implantation process inevitably results in shaving of the hair cells within the cochlea, which can result in a permanent loss of most residual natural hearing because sometimes the cause of deafness is the auditory nerve or other part of the body. While recent improvements in implant technology, and implantation techniques, promise to minimize such damage, the risk and extent of damage still varies. Still, the cause of deafness is not always identified before the surgery. It is quite possible that the surgery does not restore hearing. In addition, while the device can help the recipient better hear and understand sounds in their environment, it is not as good as the quality of sound processed by a natural cochlea. The main problem is with the age of recipient. While cochlear implants restore physical ability to hear, this does not mean the brain can learn to process and distinguish speech if the recipient has passed the critical period of adolescence. As a result, those born profoundly deaf who receive an implant as an adult can only distinguish simple sounds, such as a ringing phone vs. a doorbell, while others who receive implants early can understand speech. The success rate depends on a variety of factors, most critically the age of recipient but also the technology used and the condition of the recipient's cochlea. As the location of the cochlea is close to the facial nerve, there is a risk that the nerve may be damaged during the operation. The incidence of the damage is infrequent. An Auditory Brain Stem Implant (ABI) is a surgically implanted electronic device that provides a sense of sound to a person who is profoundly deaf, due to sensorineural hearing impairment (due to illness or injury damaging the cochlea or auditory nerve, and so precluding the use of a cochlear implant). The auditory brain stem implant uses similar technology as the cochlear implant, but instead of electrical stimulation being used to stimulate the cochlea, it is instead used to stimulate the brain stem of the recipient. Only about a thousand recipients have been implanted with an auditory brain stem implant, due to the nature of the surgery required to implant the device (as it requires brain surgery to implant the device) and the reduced effectiveness of the implant (most auditory brain stem implant recipients only have an awareness of sound - recipients won't be able to hear musical melodies, only the beat). The auditory brainstem was first implanted in humans in 1979 at the House Ear Institute, CA, USA. This original ABI consisted of two ball electrodes which were implanted near the surface of the cochlear nucleus.
III.1.Answer the questions: 1) What Is a cochlear implant? 2) What are the main parts of the cochlear implant? 3) Should a child be given a cochlear implant early or should the parent wait until later to implant the child? 4) Who gets cochlear implants? 5) How does someone receive a cochlear implant? 6) Who can use an auditory brainstem implant?
2. Make the plan of the text. Here are the titles in the wrong order. Make the order correct: 1) Cochlear implant 2) Type of hearing impairment 3) Candidates
|